In June, the FDA approved a new treatment for the most advanced type of prostate cancer. Patients who have this condition, which is called metastatic castration-resistant prostate cancer (mCRPC), have few therapeutic options, so the approval helps to fill an urgent need.
mCRPC sets in when the front-line hormonal therapies that doctors use first for treating metastatic prostate cancer stop working. These drugs limit the body’s production of testosterone, a hormone that fuels prostate cancer growth. If they are no longer effective, then doctors switch to a different class of drugs known as anti-androgens that further inhibit testosterone by blocking its cell receptor. One of those drugs is called enzalutamide.
The newly approved treatment combines enzalutamide with a second drug, talazoparib, that was already on the market for female cancer patients who test positive for BRCA mutations. These inherited gene defects boost risks for breast and ovarian cancer, but they can also elevate risks for prostate cancer in men. Indeed, an estimated 10% of men with metastatic prostate cancer are BRCA-positive.
Talazoparib inhibits a DNA-repair system called PARP that the tumor cells need to keep their own genes in working order. When PARP is blocked by treatment, the cancer cells will eventually die. Other PARP inhibitors, including olaparib and rucaparib, are already approved for advanced prostate cancer in BRCA-positive men.
During research leading to this latest approval, 399 men with mCRPC were randomly divided into two groups. One group received talazoparib plus enzalutamide; the other group was treated with enzalutamide plus placebo. The men averaged 70 years in age, and most of them had already been treated with chemotherapy and/or a different anti-androgen called abiraterone. All the men were positive for either BRCA mutations or defects affecting other DNA-repair genes.
What the study showed
Results from the still-unpublished study were presented at the 2023 American Society of Oncology Annual Meeting in June. After a median follow-up of roughly 17 months, the enzalutamide/talazoparib combination reduced the risk of death or visible signs of tumor progression by 55%.
Among the specific subgroup of BRCA-positive patients, “there was an 80% reduction in risk progression or death, which is enormous for these men and obviously very welcome,” said lead researcher Dr. Karim Fizazi, a professor at the University of Paris-Saclay in France.
Scientists had hoped that combining PARP inhibitors with anti-androgens would similarly benefit prostate cancer patients with no DNA-repair defects, but evidence from a different study by Dr. Fizazi and his colleagues shows they do not.
For that reason, the FDA approved the new combination only for mCRPC patients who test positive for mutations affecting DNA-repair genes. Dr. Fizazi and his colleagues are continuing to monitor the enrolled patients for improvements in other areas, such as overall survival, quality of life, and subsequent need for chemotherapy.
Dr. David Einstein, an assistant professor of medicine at Harvard Medical School and a medical oncologist at Beth Israel Deaconess Medical Center in Boston, says the evidence helps to confirm that PARP inhibitors have a role to play in genetically-selected men with mCRPC. Additional research is needed to assess if the observed benefits are “specific to the combination or just because access to PARP inhibition was provided at some point in the disease course,” he says.
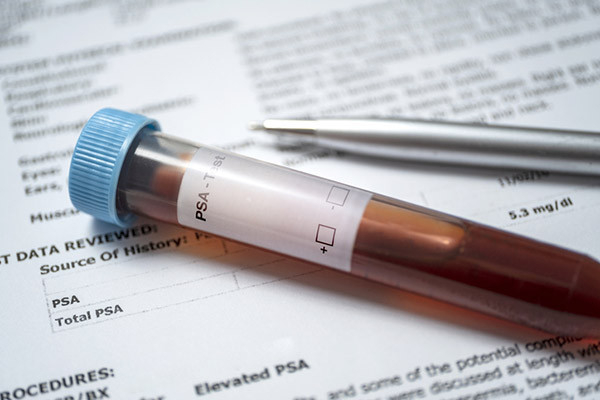
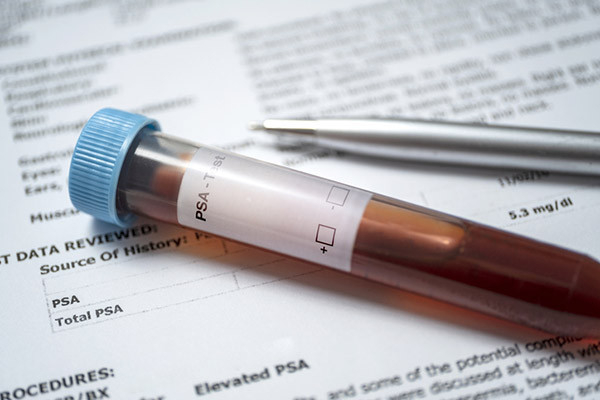
“Genetic testing for BRCA, which originally targeted females, is now becoming mainstream for men with a family history of breast and ovarian cancers, as well as men with mCRPC regardless of family history,” says Dr. Marc B. Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center. “This is important, as it has implications for other family members and treatment choices alike. Also important to note is that where this study enrolled men who had already been treated with chemotherapy and/or abiraterone, future research will likely move the enzalutamide/talazoparib combination — or components of it — to earlier disease stages.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD